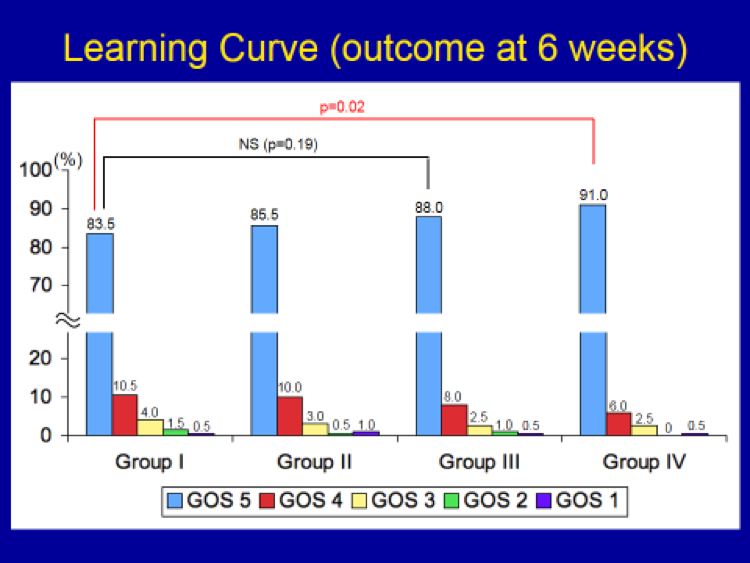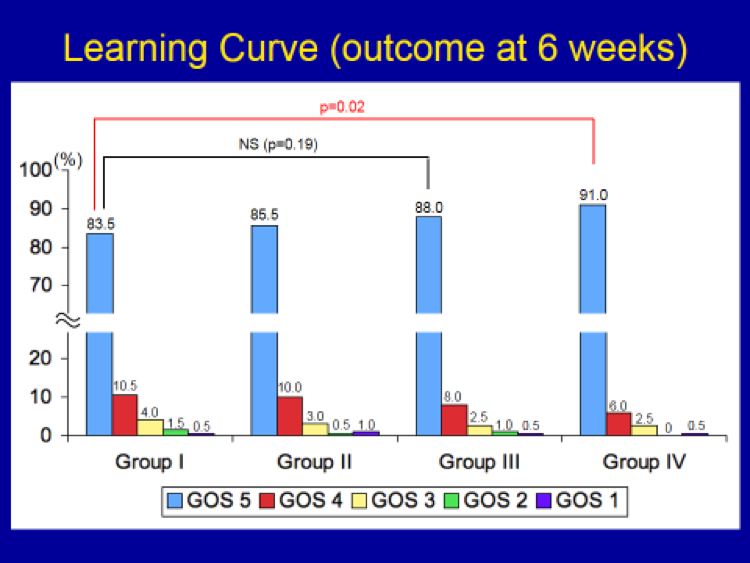
In order to see how the surgeon’s (i.e. my) experience affected outcome following meningioma surgery over time, 800 meningiomas were subdivided into groups of 200 each. The following time frame was required to accumulate the experience of 200 cases each:
Group I: 7 years
Group II: 3 years and 3 months
Group III: 2 years and 6 months
Group IV: 2 years and 6 months
There was a gradual increase in the incidence of “Normal” outcome group in each of the successive groups of 200 cases, going from 83.5 % in Group I, eventually to 91 % in Group IV. However, this difference (i.e. improvement) was not statistically significant until the last group (Group IV) of 200 cases. In other words, it takes a surgeon at least 600 cases of accumulated experience to make a statistically significant improvement in outcome in meningioma surgery. In short, surgeon’s experience is a critically important factor in determining outcome in meningioma surgery.