Surgery is considered when (1) medical therapy fails to adequately control trigeminal neuralgia, (2) patients are unable to tolerate medications’ side-effects, or (3) patients do not like the prospect of being on long-term medications.
Surgical Options:
A) Ablative (“to destroy a function by application of a noxious substance”) Surgery:
For some unknown reason, when a segment of the trigeminal nerve is “damaged” (by way of “lesioning” or “ablation” applied to it) by a noxious agent, trigeminal neuralgia pain disappears or improves. There are several surgical means of creating a focal area of “ablation” to the trigeminal nerve, and these include:
Gamma Knife (GK) Radiosurgery –
A single shot, focused radiation targeted to the trigeminal nerve
Balloon Compression Rhizotomy –
Lesioning by way of a mechanical compression to the nerve
Glycerol Rhyzotomy –
Chemical lesioning to the nerve by a type of alcohol
Radiofrequency (RF) Rhizotomy
Thermal (heat) lesioning to the nerve by RF
Long-term success rates: Glycerol 60%, Gamma Knife 65%, Balloon 67%, RF 75%
Advantages:
Short operative time (15 to 45 minutes)
Avoids general anesthesia, performed under IV sedation/local anesthetic
Good initial pain relief
Same-day procedure and quick recovery
Disadvantages:
Permanent facial numbness – RF 80%, Balloon 50%, Glycerol & GK 30%
Significant pain during surgery (performed without general anesthesia)
Need to repeat procedures due to relatively high pain recurrence rates
Indications for Ablative Surgery: (When to proceed with ablative surgery?)
- Trigeminal neuralgia patients with MS (multiple sclerosis).
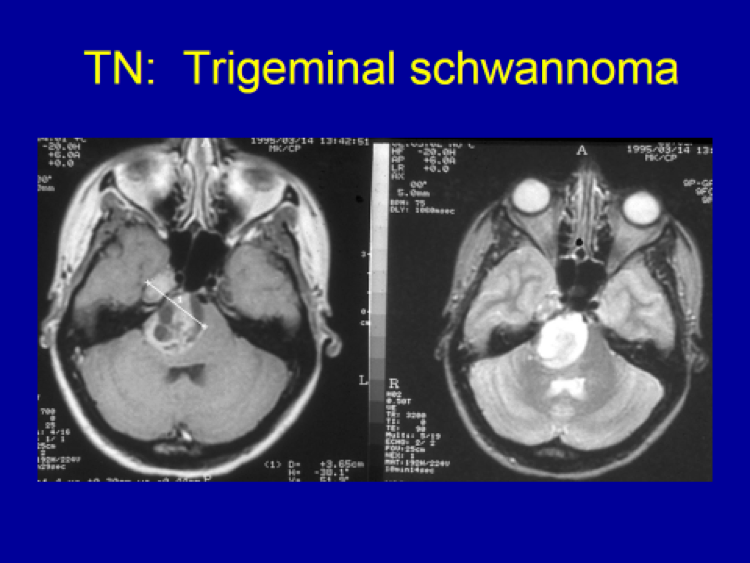
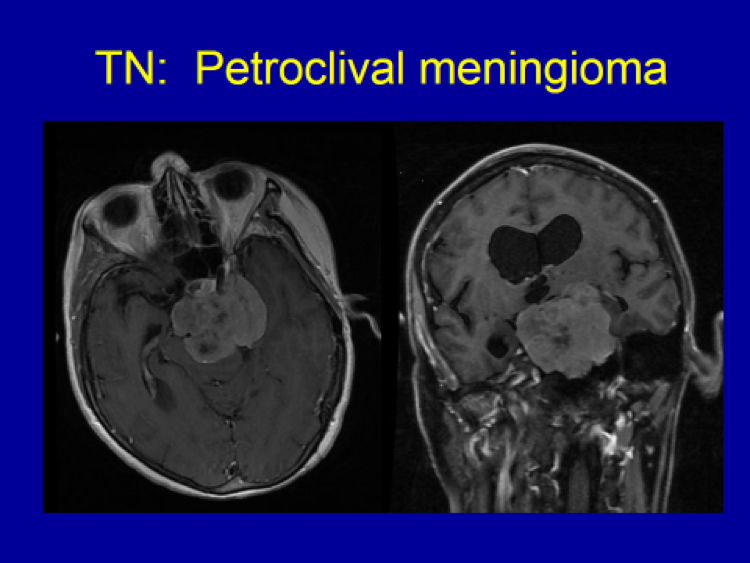
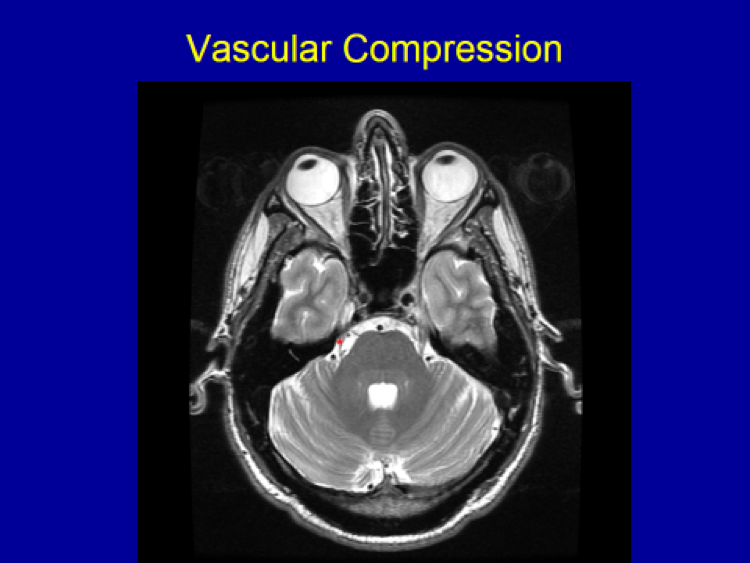
- Trigeminal neuralgia patients with no clear vascular compression on the preoperative MRI.
- Trigeminal neuralgia patients with significant medical illnesses which preclude major surgery under general anesthesia.
- Patient’s personal choice after thorough discussion of all options.
- Which specific ablative procedure to be done depends on the individual surgeon’s personal experience and choice.
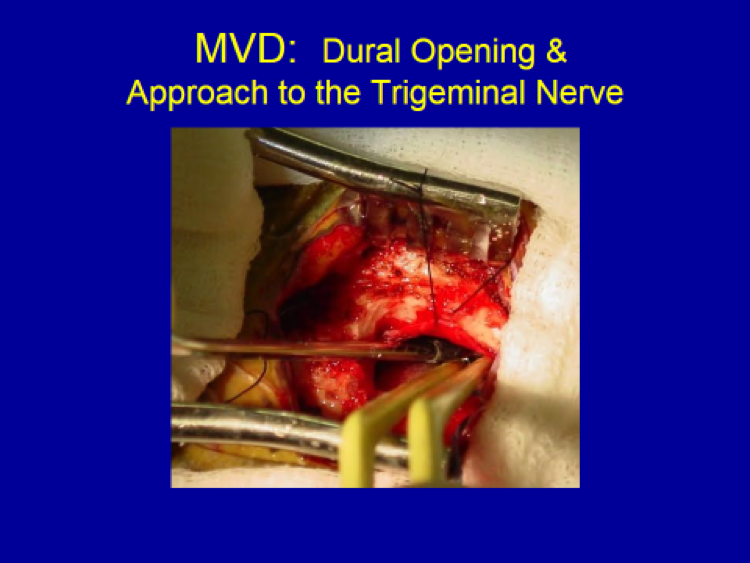
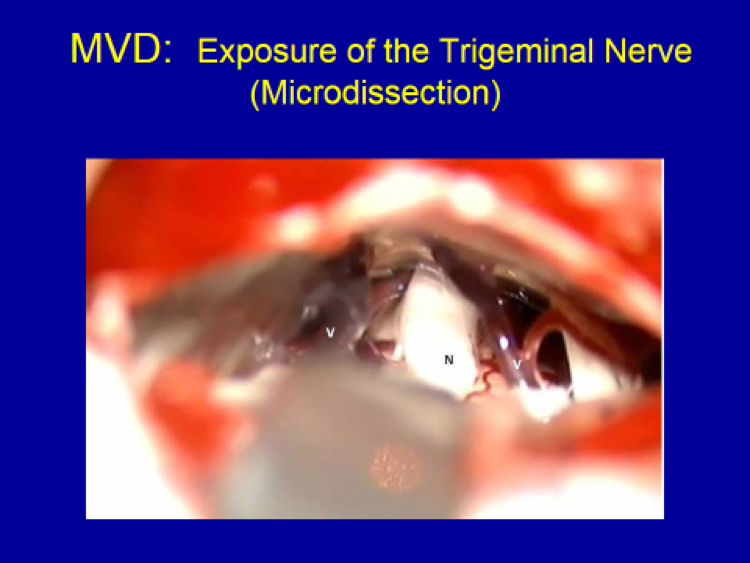
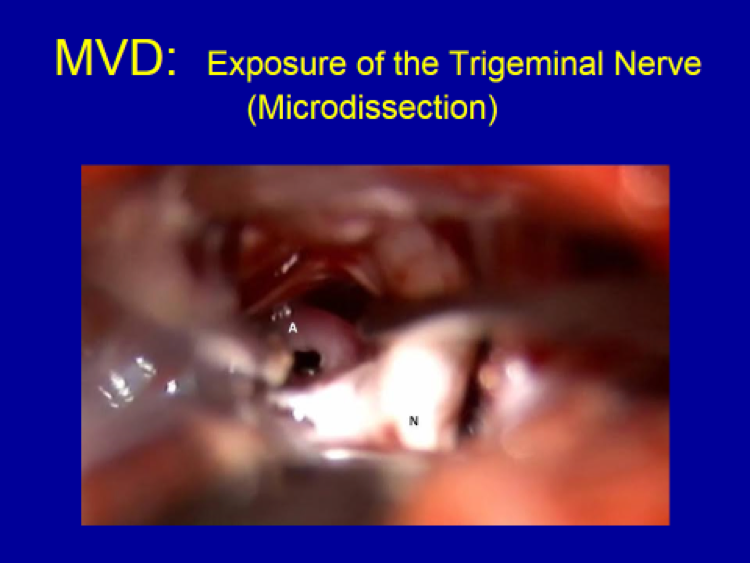
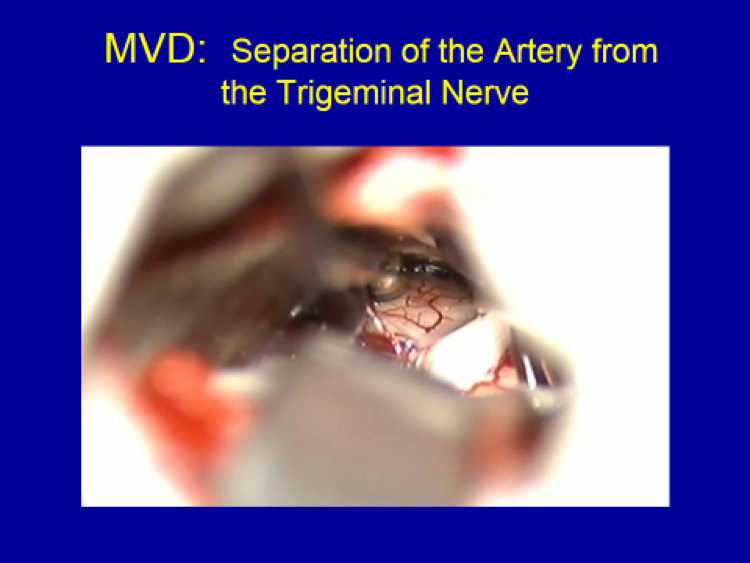
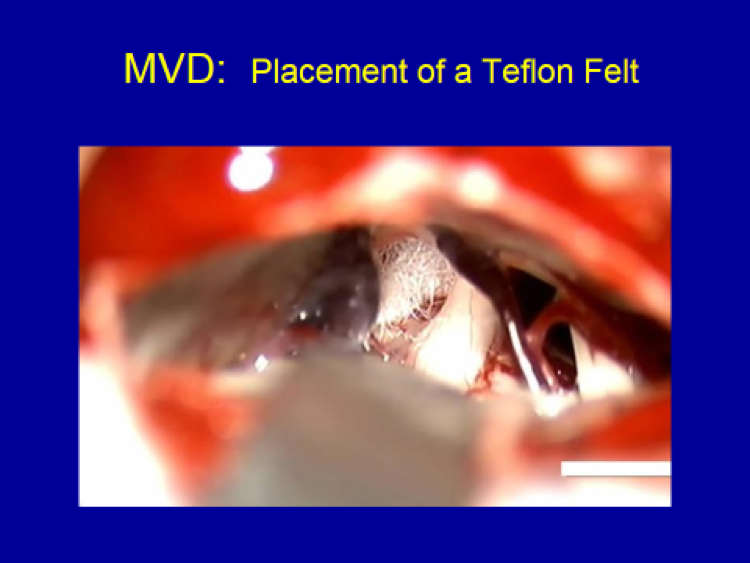
B) Non-Ablative Surgery: Microvascular Decompression (MVD)
The only non-ablative surgical technique available for trigeminal neuralgia patients is microvascular decompression (MVD).
Indications for MVD:
- Trigeminal neuralgia patients with clear vascular compression on preoperative MRI.
- Patients healthy enough to undergo 1 hour of surgery under general anesthesia.
- Patient’s personal choice after discussion of all treatment options.
Advantages:
High success rate (95% when patients are carefully selected)
Low risk of permanent facial numbness
Minimal complications (when surgeon is experienced)
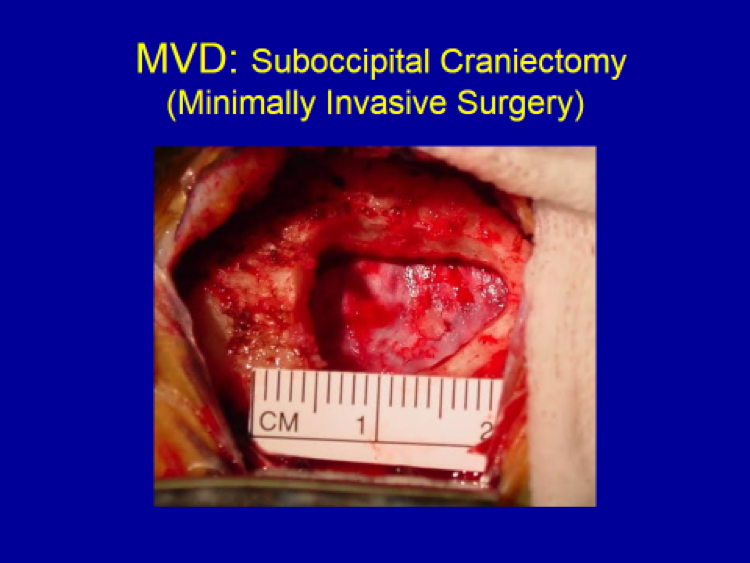
45-minutes of operative time, avoiding Foley catheter or blood transfusion
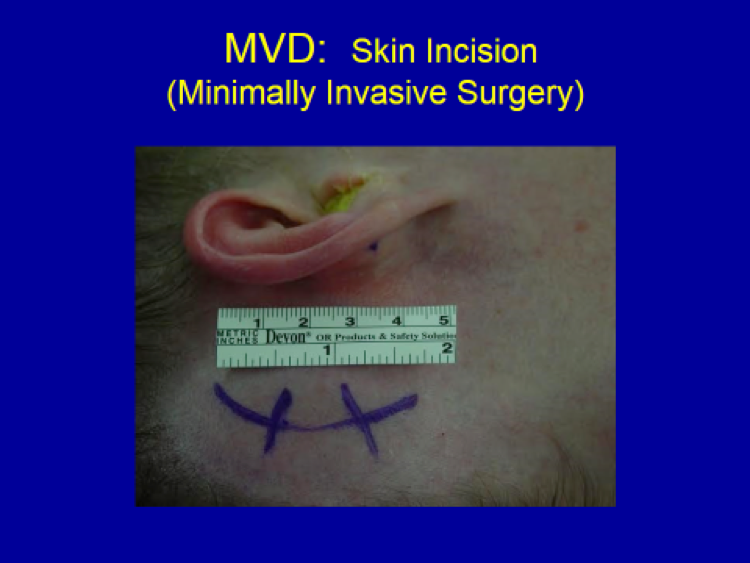
Small incision and craniotomy (bone opening)
Fast recovery (1-2 days of hospital stay)
Disadvantages:
“Brain surgery” with its associated risks (very small, but present)
Requires general anesthesia (<1 hour)
Personal Recommendation: Based on treating trigeminal neuralgia patients for nearly 30 years, my personal recommendation is MVD as it guarantees a high success rate with a low risk of permanent facial numbness. (95% success rate initially, 75-80% long-term success rate, <5% permanent numbness)